Healthcare Provider Resources
The following information about the Healthy Oregon Project (HOP) and resources on genetic screening for inherited cancer syndromes has been developed to support healthcare providers who have patients who have received results from the HOP study.
The Healthy Oregon Project (HOP) seeks to answer big scientific questions about the causes of cancer and other chronic diseases in order to save lives. Connecting Oregonians with health-related research studies, HOP combines health surveys with the voluntary collection of biological specimens (e.g., saliva). Data are stored in a secure and privacy-protected research repository. HOP is led by OHSU scientists and collaborates with researchers across OHSU and other organizations, such as the University of Oregon, and Providence Cancer Institute.
HOP is currently funded by the OHSU Knight Cancer Institute Cancer Early Detection Advanced Research Center (CEDAR). CEDAR is a research institute dedicated to identifying those at risk for cancer, detecting cancers early, and developing treatments that treat those early cancers. HOP also has the support of a growing network of collaborators.
Current collaborators include:
-
University of Oregon Center for Science Communication Research
-
Providence Cancer Institute
-
Kaiser Permanente Center for Health Research
-
Oregon Health Authority (OHA)

Are you a Healthcare Provider who would like to collaborate with HOP?
Contact our team at [email protected].
About HOP Genetic Screening
Prevention and early detection
While most cancers arise from genetic mutations acquired during a person’s lifetime, approximately 5-10% of all cancers are first triggered due to the presence of an inherited variant. Individuals with inherited cancer syndromes have an increased risk of developing cancer, often at a younger age, and, also have a higher likelihood of developing more than one cancer in their lifetime. Additionally, their siblings, children, and other family members may be at risk of having the same variant. With the advent of genetic screening, it is possible to analyze a person’s DNA and determine whether they have an inherited mutation putting them at a higher risk to develop cancer. With this information, individuals can take action earlier to prevent or identify cancer at its earliest stages when it is most curable.
No Cost
There is no cost to participate in the HOP genetic screening study for inherited cancer syndromes. Participants read about the benefits and risks of participating in the Healthy Oregon Project and consented to participate using a secure, HIPAA-compliant online portal.
Genetic screening, analysis, and reporting of results are covered by this study (including genetic counseling for anyone with a positive result).
Although most insurance companies may cover the costs of the recommended preventive measures based on having a familial gene variant, preventive care may not be covered in full. There may be out-of-pocket costs due to the patient’s deductible or copayment amount. A patient should first verify their insurance coverage before undergoing any medically recommended preventive measures.
If your patient does not have health insurance, the Participant Navigator can assist with insurance enrollment or accessing financial assistance services available in most clinics and health systems.
Positive and Negative Results Provided
Results are provided to all participants who choose this option and are ready in about four months. These reports are made available in the HOP participant’s HIPAA-compliant Healthy Oregon Project account.
HOP screens more than 30 genes associated with inherited cancer syndromes and familial hypercholesterolemia in a clinically certified CLIA laboratory at OHSU. The test is similar to but not quite as complete as testing performed by major commercial genetic testing firms. This screening test is not meant to replace clinical testing for high-risk individuals and will not detect approximately 10% of medically relevant inherited cancer risk in the genes analyzed.
When a likely pathogenic or pathogenic variant is present in these genes, the individual’s risk for cancer is likely increased over the general population. The degree of increased risk and type(s) of cancer varies between genes and variants.
The most common inherited cancer syndromes that are being screened for are:
Hereditary Breast and Ovarian Cancer (HBOC)
Families with HBOC have an increased risk for breast, ovarian, prostate, and pancreatic cancers. The genes associated with HBOC are BRCA1 and BRCA2.
More about HBOC
Hereditary breast and ovarian cancer syndrome (HBOC), predisposes women to very high risks of breast and ovarian cancer. HBOC is caused by variants in two genes, BRCA1 and BRCA2. Variants in these genes are also associated with substantially increased risks of other cancers. These genes are all involved in a specific DNA repair pathway. Effective interventions for HBOC exist. Specific recommendations on treatments and likely clinical outcomes are dependent upon the individual, the family history of cancer, and the specific variant present in these genes.
Lynch Syndrome
Families with Lynch syndrome have an increased risk for colorectal, uterine, stomach, and ovarian cancers. The genes associated with Lynch syndrome are MLH1, MSH2, EPCAM, MSH6, and PMS2.
More about Lynch Syndrome
Lynch syndrome is caused by variants in a different set of DNA repair pathway genes. The complex biology of variants in these genes is associated with a significant risk of many types of tumors, principally, colorectal and endometrial. As with HBOC, effective interventions exist and specific recommendations on treatments and outcomes are dependent on individual, family, and specific variant.
Familial Adenomatous Polyposis (FAP) and Attenuated FAP (AFAP)
Families with FAP or AFAP have an increased risk for colorectal polyps and colorectal cancer, as well as small bowel, pancreatic and thyroid cancers. FAP and AFAP are caused by pathogenic variants in the APC gene.
Cardiology Risk
We are currently screening one gene, LDLR, for pathogenic variants which are associated with Familial Hypercholesterolemia. Families with Familial Hypercholesterolemia have an increased risk for elevated cholesterol that is not manageable by a normal diet. This condition typically requires medication to decrease health risks.
Other inherited cancer syndromes are screened for on the HOP genetic screening panel, but these are much less common and the risk and cancer type(s) vary depending upon the gene and variant.
We are currently screening for changes in the following genes:
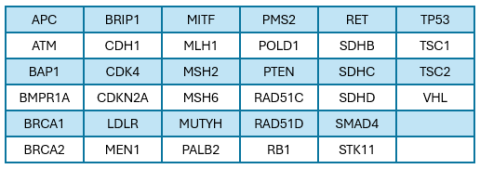
Medical guidelines may change over time as our understanding of genetics evolves. HOP only reports gene changes that have established medical guidelines that could impact clinical care. The results participants are given will be based on the current medical guidelines at the time the report is issued.
HOP is a research study that does testing that is not as complete as the testing that would be provided by standard clinical laboratories for high-risk individuals. This is because HOP’s goal is to screen participants at average risk. As such, high-risk individuals who would normally be referred to genetic counselors by their provider for standard of care should continue to be referred for formal genetics evaluation to determine cancer risk and if additional genetic testing is indicated.
If a HOP participant has a pathogenic (positive) result, an OHSU genetic counselor will contact the participant by phone to deliver the results and provide a consult to review personal and family history and review the associated cancer risks associated with the variant, medical management recommendations, and inheritance. Cancer risks and management recommendations vary by gene and variant.
Participants will receive a results packet from an OHSU genetic counselor once the genetic counselor has reviewed the result with the participant on the phone. The packet is intended for the participant and for sharing with their healthcare providers and family members. If a participant requests the report to be shared directly with their physician or others at the time of genetic consult, a release of information will be mailed to the participant to complete and return. Participants will need an OHSU Medical Record Number (MRN) in order to receive a positive result and will be assigned an MRN if they don’t have one already.
The participant will receive the information below via mail after their genetic consult:
-
copy of test result detailing the gene and pathogenic variant or likely pathogenic variant
-
result letter to summarize the consult
-
risk and management guidelines based on result and family history
-
details to share with family members about their risk and testing options
-
resources about organizations that support people with their type of inherited cancer syndrome
-
how to access the genetic counselor in the future
-
information about additional support that can be accessed through the HOP Participant Navigator.
The genetic counselor is available at any time a HOP participant has follow-up questions or concerns about their result, further genetic counseling, or screening.
For any additional questions about this study, please contact us at
[email protected]






